Researchers have proposed a significant shift in how women’s heart disease risks are assessed and managed, suggesting that evaluations and preventive treatments should begin in their 30s rather than waiting until after menopause. This recommendation comes from a new study presented at the European Society of Cardiology annual meeting in London.
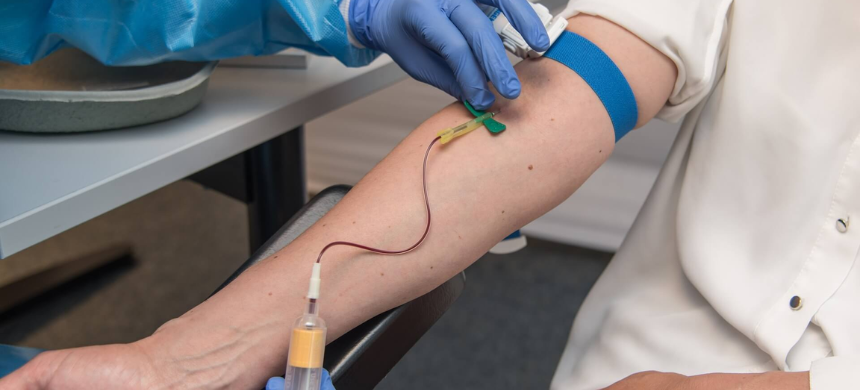
The study, led by Dr. Paul Ridker from Brigham and Women’s Hospital in Boston, highlights that simple blood tests can now estimate a woman’s risk of cardiovascular disease over the next three decades. Ridker emphasized that this information is crucial not only for patient care but also for drug manufacturers, impacting the development of cholesterol-lowering, anti-inflammatory, and lipoprotein(a)-lowering drugs.
Also Read: Huawei reveals Watch 4 with claim of first with feature of ‘high blood sugar risk’ assessment
Current guidelines generally recommend considering preventive therapies for women only in their 60s or 70s. However, Ridker argues that these guidelines need updating. “We must move beyond discussions of 5 or 10-year risk,” he said, advocating for a more proactive approach.
The study analyzed data from the Women’s Health Initiative, which involved 27,939 participants who underwent blood tests between 1992 and 1995. These tests included measurements of low-density lipoprotein cholesterol (LDL-C or “bad cholesterol”), high-sensitivity C-reactive protein (hsCRP), and lipoprotein(a), a genetically determined type of fat.
Results showed that women with the highest levels of these markers had significantly higher risks of major cardiovascular events. Specifically, women with the highest levels of LDL-C had a 36% increased risk, those with the highest hsCRP levels had a 70% increased risk, and those with high lipoprotein(a) levels had a 33% increased risk of cardiovascular events over the next 30 years.
Moreover, women who had high levels of all three markers were found to be 2.6 times more likely to experience a major cardiovascular event and 3.7 times more likely to suffer a stroke in the coming three decades.
Ridker noted that these biomarkers are independent of each other and provide distinct insights into the different biological issues each woman may face.